One of the most common medical disorders occurring during pregnancy is iron deficiency anaemia. Indeed, it is so common that all pregnant women in Anguilla are screened for it at their first visit to their obstetrician or midwife. Fortunately, if diagnosed early it can be successfully treated and many complications prevented.
What is anaemia in pregnancy?
During pregnancy the body’s demand for iron is greater. Iron is needed in pregnancy for the developing fetus’ growth and brain development.
Iron deficiency anaemia during pregnancy results in a reduction of red blood cells which help to transport oxygen around the body.
To produce red blood cells, the body needs iron, vitamin B12 and folic acid. If there is a lack of one or more of these, anaemia will develop. The most common type of anaemia in pregnancy is iron-deficiency anaemia.
Risk factors for anaemia in pregnancy
All pregnant women are at risk of becoming anaemic. That is because they need more iron and folic acid than usual, but the risk is higher if you:
• Are pregnant with multiples (more than one child)
• Have had two pregnancies close together
• Vomit a lot because of morning sickness
• Are a pregnant teenager
• Do not eat enough foods that are rich in iron
• Had anaemia before you became pregnant
Symptoms of iron deficiency anaemia in pregnancy
Symptoms might be varied and might resemble the symptoms of pregnancy. The most common symptoms of iron deficiency anaemia in pregnancy include the following:
• tiredness and lack of energy
• shortness of breath
• noticeable heartbeats (heart palpitations)
• pale skin
Diagnosis
Following a general examination, your doctor will arrange a number of blood tests. The diagnosis can then be made and treatment commenced.
Treatment
Once a diagnosis is made your obstetrician or midwife will discuss with the pregnant woman how her anaemia will be treated.
Iron supplements are available in tablets or in a liquid form. If you have been prescribed iron supplements, it is important to take them and to finish the course. You will then be offered a blood test to check that the iron supplement has been beneficial. If you fail to respond to iron supplements, intravenous iron may be considered – however there can be risks with this.
Iron supplements can often cause constipation or diarrhoea and some women are unable to take them. Iron supplements are better absorbed if taken an hour before meals, however, side effects on the gut, such as abdominal discomfort, constipation, diarrhoea and nausea can occur. Some of these symptoms may be resolved by taking the iron with or after food. Please talk to your doctor or midwife about this.
If iron deficiency anaemia is only diagnosed very late in the pregnancy a transfusion of red blood cells might be needed. If the pregnant woman was having regular prenatal visits this form of treatment should not be needed as it has its own risks.
Complications
Severe or untreated iron deficiency anaemia during pregnancy can increase the pregnant woman’s risk of having:
• A preterm or low-birth-weight baby
• A blood transfusion (if you lose a significant amount of blood during delivery)
• Postpartum depression
• A baby with anaemia
• A child with developmental delays
How can I avoid anaemia whilst I am pregnant?
Paying special attention to your diet is important in preventing iron deficiency in pregnancy. Pregnant women are encouraged to eat the following. Iron-rich foods:
• Dark-green leafy vegetables, such as kale
• Iron-fortified cereals or bread
• Brown rice
• Pulses and beans
• Nuts and seeds
• White and red meat
• Fish
• Eggs (these must be well cooked during pregnancy)
• Dried fruit such as dried apricots, prunes and raisins.
A pregnant woman’s daily diet should include foods from all the major food groups to ensure it’s healthy and balanced. It is important to be aware that foods contain vitamin C are important as vitamin C helps your body absorb iron. The following are a good source of vitamin C: fresh fruit juices, tomatoes, peppers, broccoli and potatoes.
Consuming large amounts of some foods and drinks, as well as certain medicines, may make it harder for your body to absorb iron. These include tea and coffee, calcium, and antacids.
Conclusion
Iron deficiency anaemia is one of the most common causes of anaemia in pregnant women. Once the diagnosis of iron deficiency anaemia is made, oral iron supplements is usually the most common form of treatment. Attention to a balanced diet is key to preventing and treating iron deficiency anaemia in pregnancy. Once treatment is commenced many of the complications associated with severe iron deficiency anaemia in pregnancy can be prevented.
Ask Your Dr is a health education column and is not a substitute for medical advice from your physician. The reader should consult his or her physician for specific information concerning specific medical conditions. While all reasonable efforts have been made to ensure that all information presented is accurate, as research and development in the medical field are ongoing, it is possible that new findings may supersede some data presented.
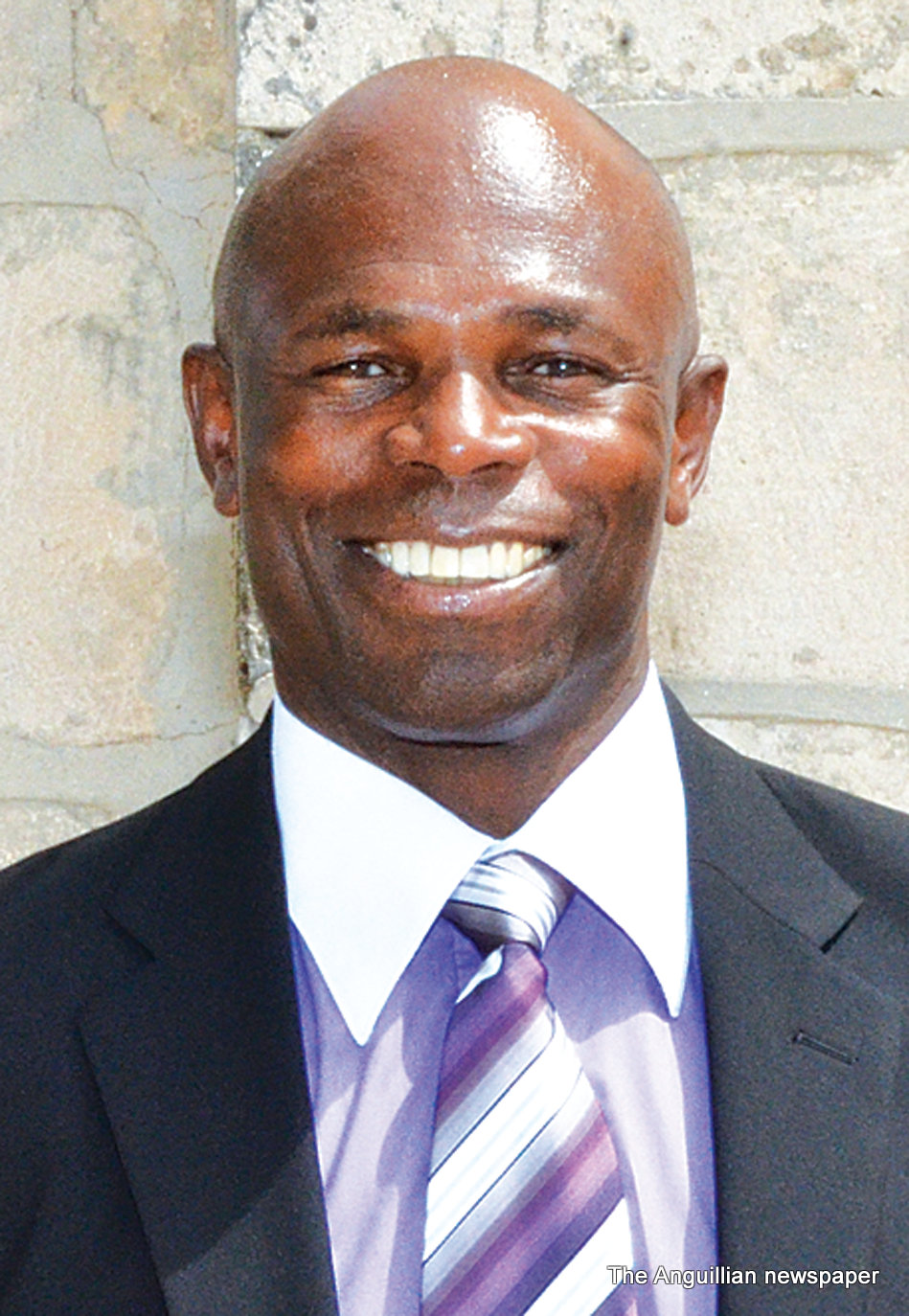
Dr Brett Hodge MB BS DGO MRCOG is an obstetrician/Gynaecologist and Family Doctor with over thirty-six years in clinical practice. Dr Brett Hodge has a medical practice in The Johnson Building in The Valley (Tel: 264 497 5828).